
When treatment began, Rina Ranalli managed every bite of food that entered her 13-year-old daughter’s mouth. For 2 1/2 months, she prepared three meals a day, plus two snacks, each packed with the calories and fats her daughter’s anorexic, malnourished body desperately needed. Cream was poured into almost everything.
But convincing her daughter -- who had gone from being a healthy 7th-grader to a girl who secretly threw away her lunches and lost 15 pounds in six weeks -- to eat was often a Herculean battle.
Some days, her daughter yelled. Other days she was resigned. But in those early stages, every meal Ranalli served her daughter at the kitchen table of their Chicago home was colored by her daughter’s extreme anxiety about eating. "You can see how terrified your child is, that life has become a never-ending treadmill of being obsessed by food, but not letting a piece into your mouth," Ranalli said. "You’re there saying over and over in as calm and reassuring a way as you can, 'This is your medicine, you need this.'"
This is the day-in, day-out of phase one of the Maudsley method for the treatment of anorexia, also known as family-based therapy. The intensive outpatient approach, which was developed in the 1980s at the Maudsley Hospital in South London, breaks with more traditional anorexia treatments in that it requires parents -- not professionals running residential facilities -- to take complete control of their children’s eating, before slowly turning it back over to them.
A DIFFERENT APPROACH
"With just about every other illness, psychiatric or medical, parents are always seen as a resource to help their kids,” said Daniel Le Grange, director of the eating disorders program at The University of Chicago and a pioneer of family-based therapy. "With anorexia treatment, for some reason, we have excluded parents,” he said. “This treatment is telling parents, 'You can do this.'"
Some estimates suggest that up to 20 percent of people with anorexia -- 85 to 90 percent of whom are girls and women -- will die, making it the deadliest mental health condition, and one that disproportionately affects tweens and teens. According to the National Association of Anorexia Nervosa and Associated Disorders, 95 percent of eating disorder sufferers are between the ages of 12 and 26, and anorexia is the third-most common chronic illness in adolescents. But while much is known about the prevalence of eating disorders and which groups are at high risk for them, relatively little is known about the disorders' causes -- making them extremely difficult to treat.
Between 1999 and 2006, the rates of hospitalization for anorexia increased by 17 percent, according to the Healthcare Cost and Utilization Project. At least one study, published in the Journal of Adolescent Health in February, has questioned the efficacy of hospital refeeding protocols -- saying they may not be sufficiently aggressive. The diets generally start with just a small number of calories and “may be too conservative to produce a rapid and significant weight gain,” the researchers wrote. “This could result in lower discharge weight or prolonged hospital course.”
Maudsley advocates say that even when hospitals and residential facilities successfully help a child re-establish a safe weight, they may not adequately prepare parents for the significant, ongoing burden of helping that child maintain their weight at home.
“Nobody gets cured of an eating disorder, by and large, in a residential place. You may get the weight on, and you may get some attitude adjustment, and some people then are fine,” said Dr. Russell Marx, chief science officer at the National Eating Disorders Association. But for many children and teens with anorexia, “there’s going to be a gravitational pull back to the illness at first,” he said.
HOW IT WORKS
With family-based treatment like the Maudsley method, parents control the refeeding. Patients go through three distinct phases, with the help of a psychiatrist, psychologist, social worker or other mental health professional who has been trained in the method and who generally conducts between 15 and 20 sessions with a family over at least six months. Phase one focuses solely on weight restoration, and parents take total control over what their child eats -- not unlike what a nurse might do in an inpatient treatment program. The goal is to counteract the most pressing and dangerous effects of anorexia -- malnutrition, dehydration, as well as potentially fatal changes to the heart and immune system --- as soon as possible.
In phase two, parents gradually hand control of feeding back to their son or daughter. Phase three begins when the teen has stopped restricting food. It focuses on long-term strategies for managing the disease and on some of the psychological and family factors underlying the child’s illness -- a step that’s taken much earlier in many traditional residential programs.
Claire, who has blogged about her experience as a Maudsley parent, believes that the method has been essential to her daughter Lauren’s success. When Lauren was a sophomore in college, she started on a diet that quickly became full-blown anorexia. Claire, her husband and Lauren attended an intensive five-day, multi-family treatment program at the University of California San Diego, which cost $5,000, 60 percent of which was covered by their insurance. Claire said the process of helping her daughter eat again was grueling -- in the beginning, Lauren was supervised not just during every meal and snack, but for up to an hour after. But success came with perseverance, Claire said, with telling Lauren over and over: It’s not an option not to eat.
Story continues below photo.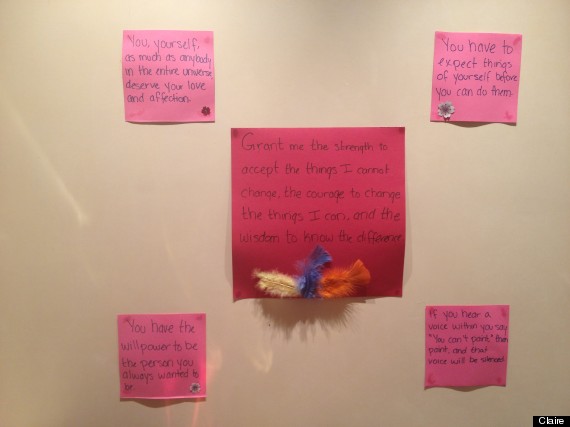
Inspirational quotes Lauren keeps in her room at home. The act of creating them was also helpful, because crafts were a good distraction while she was in recovery, her mom, Claire, said.
Perhaps the biggest challenge for Claire was knowing when it was safe to take a chance and move forward through the program’s phases with a daughter who was eager to assert her independence. “When she left home and returned to college, it was absolutely wonderful, on the one hand, but it was still scary because we didn’t know how she would do there,” she said. “But there is no way of knowing without trying.”
A contract that Claire, her daughter and her husband developed together early on in the program was a rock the family clung to, Claire said. It stipulated that if Lauren slipped below the healthy weight range established during the treatment program in San Diego, or if she failed to attend regular therapy sessions, then she would have to come home from college indefinitely.
Lauren graduated from college last spring, has a job and is living independently. She and her family are slowly transitioning away from the contract, and hope that someday soon they won’t need it at all. But one of the biggest challenges in eating disorder treatment is that there is no clear definition of what complete recovery means. For her part, Claire defines it as the absence of all “eating disorder behavior and thoughts.” “We would consider the treatment to be, overall, very successful because she hasn’t had a relapse,” she said. “I think her prognosis is good, but she’s still vulnerable.”
NOT FOR EVERYONE
Only a handful of randomized, clinical trials have been published on eating disorder treatment in adolescents of any kind, but those focused on family-based therapy support its efficacy. A 2010 study in JAMA Psychiatry (formerly the Archives of General Psychiatry) comparing the Maudsley method to adolescent-focused therapy -- which consists largely of one-on-one sessions addressing issues underlying the eating disorder -- found that the two had similar results when treatment ended, but that Maudsley had better remission rates at 6 and 12 months out.
“There’s a cautious consensus that family-based therapy should be the first-line treatment for medically stable patients,” said Le Grange, who was an author on the paper.
But the major studies that have examined Maudsley have all been relatively small. The JAMA investigation, for example, included only 120 participants. On the whole, Marx said, the success rates for family-based therapy hover somewhere between roughly 50 and 70 percent, depending on whom you ask.
Family-based therapy may not be an option for many families simply because of the time it demands from parents. During the first two weeks, the patient doesn’t go to school, and one parent must be available around the clock to feed and observe their child, Le Grange explained. As the program progresses, it does allow families some flexibility in how they live day-to-day -- a grandparent or willing family friend could step into the enforcer role, for example. However, the time it requires may well put the treatment out of reach for families who can’t afford to take time off from work.
“I was lucky in that I was a stay-at-home mom at the time … and I had a very supportive, loving husband who would say, ‘I will take this meal,’” Ranalli said. “If you’re doing three meals, and three snacks, it feels like mealtime is all the time … you’re at that table a lot.”
Yet despite such logistical challenges, interest in family-based therapy continues to grow. In 2006, the treatment was given a huge boost thanks to a New York Times story by Harriet Brown, a journalist whose daughter “Kitty” (her family nickname), was treated with the method. When the piece was published, Brown teamed with a few other Maudsley moms she’d met on various eating disorder support websites and launched Maudsley Parents, a site that provides information about the method. Brown, who has since written a book about her family’s experience with Maudsley, called Brave Girl Eating, said that awareness about the method is still relatively limited.
“Back in 2006 when I started talking about this stuff, family-based therapy was considered more of a crackpot theory,” said Brown. “I do think that has changed. If you call the National Eating Disorders Association helpline and say that you have a child under 18 with [anorexia], they direct you to our website [as a possible source], which they certainly did not do in 2006.”
Brown, and other Maudsley believers like Ranalli, say the method gave them what they could not find at a time when their children’s illness had rocked them to the core: a sense of empowerment. By foisting the onus almost entirely on Ranalli and her husband, the program bolstered her belief that she could save her daughter -- a confidence that was absent during the months she floundered with a well-meaning nutritionist and a more traditional counselor, begging her daughter to eat.
Ranalli recalls one wrenching encounter when the nutritionist gave her daughter a container with peanut butter and apples. Her daughter took it and promptly split it in half -- because the package said it had two servings. She refused to eat the whole thing. It was, Ranalli said, the moment she realized that there was no sanity there, only disease.
“My daughter couldn’t see that she was starving, that she needed the other half,” Ranalli said. “When I went to Maudsley, they said, ‘You, as a parent, you know what your child needs.’”
