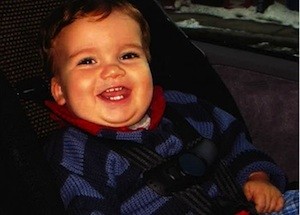
Everly Macario recalls the "primal shriek" her son released one fateful April morning in 2004. By the end of the day, Simon Sparrow, who had not yet turned 2, would succumb to an increasingly common infection called methicillin-resistant Staphylococcus aureus (MRSA).
MRSA may have been the official cause of death, but Macario suggested that Simon really died as a "direct result of all of us misusing and overusing antibiotics" in both humans and food animals. Macario joins 30-some parents, pediatricians and organic farmers as part of the group Supermoms Against Superbugs, who are converging on Capitol Hill Tuesday to ask the federal government to rein in the use of antibiotics in agriculture, in hopes of preserving the efficacy of antibiotics and protecting children's health.
"Yes, doctors are overprescribing. That has contributed," added Macario, who is also co-founder of the MRSA Research Center. "But now the Mount Everest challenge is to get farmers to stop using antibiotics in animal feed and water."
According to the latest estimates from the U.S. Food and Drug Administration, 80 percent of antibiotics are given to food animals -- with the majority of those used for growth promotion or disease prevention rather than for treatment. Overall, the more antibiotics used, experts warn, the more microbes become resistant to those drugs -- and the more people may be exposed to drug residues and drug-resistant genes in their food, water and the environment. It's survival of the fittest at a microscopic level.
Compounding the issue is the ability of bacteria to share their drug-evasion secrets with one another while mingling in an animal's or human's gut, in a swine feces lagoon or in a river. For example, even if a particular drug-resistant microbe isn't capable of causing illness in humans itself, its DNA could find its way into more malignant microbes that might infect a child.
Despite the progress that's been made in limiting unnecessary antibiotic use in humans, Dr. Cecilia Di Pentima, an infectious disease pediatrician at Vanderbilt University, shares Macario's broader concerns. "We're failing as a society in preserving antibiotics," she said, "and we're paying for it."
Di Pentima has also joined Supermoms Against Superbugs in D.C. to share the tragic ramifications she witnesses first-hand in her daily practice -- from MRSA to other dangerous infections, such as vancomycin-resistant Enterococcus and multi-drug resistant, gram-negative bacteria.
"For us, it's a daily struggle with very sick kids," said Di Pentima. "Even healthy kids who have never been in a hospital can come in with infections resistant to almost all antibiotics."
She and other doctors now frequently resort to either higher doses of drugs, more toxic drugs or both. Di Pentima said that she is seeing increased rates of kidney failure as a result. In the worst cases, like Simon's, there might be no alternatives at all.
Ruby Lee of Troutdale, Ore., was only 10 months old when she got sick after eating ground turkey meatballs infected with a form of salmonella resistant to multiple antibiotics. Fortunately, her doctor eventually found an antibiotic, cephalosporin, that effectively defeated the bacteria and saved her life. Ruby's mother, Melissa Lee, is also among the group visiting today with the FDA, the U.S. Department of Health and Human Services and the White House. She, too, wants to ensure that other families don't have to suffer as hers did.
In January, the FDA prohibited certain uses of cephalosporins in cattle, swine, chickens and turkeys. The move was welcomed by advocates, who also suggested that it was not nearly enough to combat the overall rise in antibiotic-resistant superbugs.
A similarly contentious response was sparked when the FDA released guidelines last month that asks pork, beef and poultry producers to stop using antibiotics voluntarily for fattening up their livestock.
Those guidelines still allow broad use in animals for disease prevention, noted Laura Rogers, project director for the Pew Campaign on Human Health and Industrial Farming, which organized today's event alongside the American Academy of Pediatrics. "Oftentimes dosages for prevention are the same as those used for growth promotion," she said. "If we just call it something else, we won't see drug use go down."
Other regulatory targets for advocates include the Preservation of Antibiotics for Medical Treatment Act, which was re-introduced in March 2011 after getting buried in Congress in 2007 and 2009, as well as a recent order from a federal court that the FDA follow through on a rule proposed in 1977 to withdraw approvals for most non-therapeutic uses of penicillin and tetracyclines in livestock -- both drugs crucial in human medicine.
"We're going to ask whoever we meet with on Capitol Hill to help support legislation that will reduce misuse and overuse of antibiotics in industrial food animal farms, because that is contributing to antibiotic resistance in a major way," Macario said. "If we don't do something about it, more children are going to die. That's a fact."
In addition to participating with the Supermoms virtually via Facebook and Twitter, Macario also reminds parents of their ability to influence change at home.
"They can make their voices heard by buying meat and eggs that originated at farms that don't use antibiotics, and when they go to restaurants, they can demand food raised without antibiotics," she said. "Ultimately, consumer demand is going to drive change."
