Personalization is threaded into the social fabric of America. Innovation is rooted in customizing and personalizing even the smallest parts of our lives, stemming from technology and retail to travel, media and wellness. The future continues to promise even smarter applications where personalization fits, but what about our health? Enter, precision medicine -- this new era of personalized medicine has arrived to healthcare and the possibilities in treating cancer unimaginable just a few years ago, are closer than ever. Imagine a world where your treatment was tailored to you, taking into consideration every cell and gene throughout your individual genetic profile, using that data to specifically design a treatment to fight the exact cancer you have? Sound too good to be true? Think again. The future is here, and the healthcare industry is preparing for massive disruption but for once disruption couldn't have come at a better time.
The Road to Personalized Medicine for Cancer Treatment
For decades, physicians had the same approach for all patients with the same type of cancer, be it breast, lung, liver or prostate cancer, the same way, even through they were aware drug treatments may work on some and fail in others. This is not to say all cancers are treated the same, but the basic approach and process is used when it comes to diagnosing, staging, and recurrence. As significant advances in research progressed over the course of the last 30 years, the medical community created standards of care and treatment when it came to diseases like diabetes, heart disease, and even cancer. However, treating cancer cannot be classified with a standard approach. What we're learning more and more comes down to the individual. Each person is as unique on the inside as they are on the outside. Therefore, why wouldn't we treat their cancer using an individual approach?
For the last 20 years, cancer cells have outsmarted us by protecting themselves, building a wall, not allowing the immune system to identify and kill them. Current treatments are not aimed at stopping cells from spreading and have almost no selective capacity to distinguish between cancer cells and healthy cells. We've basically poisoned the body to kill cancer using chemotherapy and even radiation. But advancements in research has led to a number of potential targeted therapies designed to fight cancer, among them one approach is gaining more and more support -- immunotherapy. This type of targeted therapy teaches our own immune system to fight cancer cells and spare healthy ones. By injecting bacteria inside cancer cells and putting them back into the body, the immune system can learn to recognize and kill them. Think of your T cells as guided missiles aimed at killing the bad cancer cells versus a bomb that kills every cell in its path such as chemotherapy. But an approach we could've never foreseen 10 years ago is right around the corner, leading a transition not just from the diagnosis and treatment of these cancers but much more emphasis on prediction and prevention.
Welcome to the world of precision medicine also deemed "personalized medicine," where each patient is treated individually based on their genetic makeup and the specific genetic mutations present in their body. The National Institutes of Health defines precision medicine as an emerging approach for disease treatment and prevention that integrates an individual's variability in genes, environment and lifestyle. To take it even further, precision health may be the new approach to medicine, rooted in prevention and prediction of various diseases while also maintaining overall health and quality of life.
In my field, which is prostate cancer, we talk a lot about an individual patient's risk factors such as family history, which is a huge proponent of the disease and how aggressive it is. While oftentimes surgery is the first line of defense, the right way to treat prostate cancer and any cancer is through individualized care. Recently at the 110th Annual Scientific Meeting of the American Urological Association, a significant study was presented which showed a combined assessment of genetic bio markers and the genetic profile for a patient would lead to better methods for diagnosing, treating and measuring the likelihood of the disease recurring. The breakthrough here is the role genetic testing plays in cancer, throughout the entire process, from diagnosis to recurrence. We can gather more information about the patient at each step of the way.
Precision Medicine Meets Individualized Care
I've always spoken about the importance of individualized care, especially when it comes to diagnosing and treating cancer. Innovations in genomic testing are leading this emerging era of cancer therapy -- analyzing a group of genes and their activity, which can influence how a cancerous tumor is likely to grow and respond to treatment. This type of diagnostic testing analyzes and detects very specific abnormalities in the tumor cells in a patient's individual cancer. Unlocking the mysteries of genetics holds the promise of finding more customized cures with drugs that attack genetic mutations or repair genetic defects based on the individual patient. Advances in genetic sequencing has increased the likelihood of detecting mutations driving tumor growth and even specific cells inside the tumor. This is the future of treating and diagnosing cancer, integrated with the promise of precision medicine.
Is this revolutionizing everything we know about cancer, from prevention and diagnosis to treatment and recurrence? I would say yes. We've always identified cancer based on the organ it originates in such as the prostate, colon or liver, grouping these together as if they grow the same. What we know now is just because it's deemed "prostate cancer" doesn't mean all prostate cancers develop or progress in the same way. Testing the genetics of an individual patient has opened up an entire new conversation in oncology leading us to define within the cancer what actually drives its development and progression.
The Precision Medicine Initiative
- More and better treatments for cancer
- Creation of a voluntary national research cohort
- Commitment to protecting privacy of patient volunteers to participate in the studies
- Regulatory modernization based on this new research and care model, including changes needed to privacy and participant protection framework
- Public-private partnerships across existing research cohorts, patient groups, and private sector to develop infrastructure needed to expand cancer genomics and launch a voluntary million-person cohort
It is indeed a massive initiative but perhaps just what we need to make big changes to approaching and treating cancer, which is projected to increase 55 percent by the year 2030, with 22 million cases in the United States.
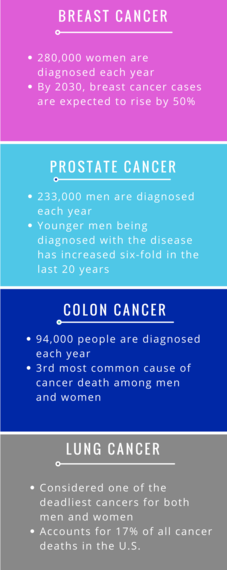
Four of the most common cancers in America are lung, breast, prostate and colon cancer among men and women. Lung cancer being one of the deadliest, accounts for 17 percent of total cancer deaths in the U.S. Over 792,295 people are diagnosed each year. Colon cancer affects almost 94,000 people each year and is the third most common type of cancer and second leading cause of cancer death in men and women with almost 50,000 dying each year. U.S. cases of breast cancer are projected to rise 50 percent by 2030 totaling to 441,000 cases per year. It's the most common type of cancer in women currently with 280,000 new cases each year. Lastly, for men prostate cancer is the second leading cause of cancer death in the U.S. Known as the silent killer since there are little to no symptoms in the early stages, it's continuing to be very prevalent among younger men. If it occurs in men age 50 or younger, it's likely because the tumor is growing rapidly, making for a much more aggressive cancer.
Genomic testing and precision medicine also have the potential to make a huge impact on the diabetes epidemic in this country. Over 86 million Americans suffer from pre-diabetes which even in the pre-stages can lead to cardiovascular diseases. 29.1 million people have diabetes and the full impact of the disease on a person's life is much larger, leading to cause of death often being from heart disease or kidney failure.
Imagine a world where treating cancer and other chronic diseases like diabetes is customized to your specific case? The possibilities of better treatments and even finding a cure is even closer with precision medicine and genomic testing. It's amazing to think that with this approach, we could identify a person's risk factors extremely early in their life and even prevent some of these diseases from developing. What a concept that is. Are we closer to a cure for cancer? I think it's safe to say we're closer than ever before.