Not too long ago, I had to make an appointment for a family member with a specialist at a large academic medical center in New York City. The referral was made by a community doctor as a result of certain concerns raised by the doctor about the results of various tests and scans. After a week of leaving messages and talking to four different people at this medical center, I was told that the earliest the doctor could see us would be in October. October! And here we are in August!
These types of scenarios make it hard to believe that anyone in the medical community is thinking about the patient and the emotional and psychological implications of waiting more than two months to see a doctor when concerns have been raised about a patient's medical condition. It is hard to believe that things were ever different, and yet they were.
Recently, I was invited to give a TEDx Talk with UC Davis in San Francisco on the subject of Redefining Normal and I took a look at health care -- where we were, where we are and where we're going. Remember when we had family physicians? A doctor would come into our homes to treat us and our entire family. Doctors knew us -- our circumstances, our family, our financial pressures and medical history and our overall lifestyles. Things began to change radically with the institutionalization of health care that occurred over the past several decades.
The emergence of Medicare, Medicaid, labor unions, private insurance companies, etc. resulted in care being based on formulas -- not individuals. Likewise, the significant medical and scientific advances in screening, testing and treatments have no doubt saved countless lives but further distanced patients from their doctors and health care team. We know much more about a patient today than at any time in our past but have forgotten that sometimes what matters most is actually what the patient has to say.
Today, we are living in a time of change. There are a growing number of examples of the health care system bending towards the needs and wants of the patient. Walk-in clinics are a good example -- fast, easy, open early, late and on the weekends. On a policy level, The Affordable Care Act has mandated the formation of the Patient-Centered Outcomes Research Institute (PCORI), examining different models of patient-centered care and how they can improve quality and decrease cost. And we are witnessing a proliferation of health-related apps allowing consumers to track their own health, wellness and medical information. There is an all-around push across health care for a new model of "patient centered care" where the individual voice matters again.
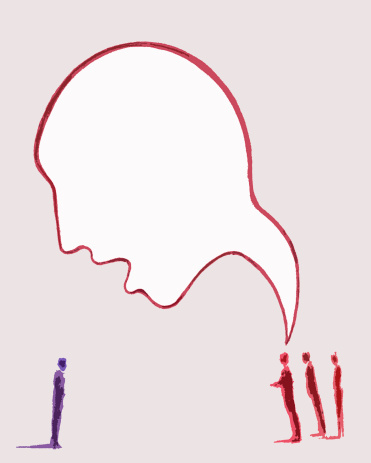
And yet, as the system is evolving towards true patient-centered care, and patients are becoming more and more involved in decision-making, few patients are actually prepared for this new model.
At the Cancer Support Community ("CSC"), we have a program called Open to Options. Through this free program, a patient can talk to a trained Decision Counselor when they are confronted with any medical decision -- whether to choose Treatment A versus Treatment B, a mastectomy versus a lumpectomy, or perhaps whether to enter a clinical trial. The Decision Counselors help the patient raise his/her voice by developing a question list and insert his or her own preferences and values into the equation.
Usually, the doctor is looking at medical data, outcomes, and efficacy and recommending treatments that will lead to the best survival for the patient. But patients tell us that life is about so much more than "surviving" -- it is about living! Patients want to know, "How will this impact my quality of life -- my mobility, my independence, my ability to enjoy friends and family?" "What will the cost of this treatment course be for me and my family versus other treatments?" "Will I get a placebo in a cancer clinical trial?"
Yet for all the progress I have seen on the individual patient front, questions continue to linger. "How do we better integrate these types of interventions that really matter for patients into mainstream medical care?" "How do we make sure integrated care -- including counseling, decision-making, patient education, comprehensive care planning -- is mandated, integrated and paid for?" These are things we know matter to patients. How do we ensure that the patient voice is raised -- and heard? We tackled the institutional deaf ear by creating an outlet for the collective Patient Voice, our Cancer Experience Registry in which nearly 10,000 patients with cancer and cancer survivors have shared information about their experience and needs throughout the cancer journey.
The data has been valuable in identifying gaps in care as well as leading to new programs and services to address those gaps. It has revealed that while there are some consistent themes across the various diagnoses, people with different kinds of cancer have issues that are more specific, or even unique to their individual diseases. For example, a growing number of patients are experiencing their cancers as a chronic condition over the course of years. This trend means that people impacted by cancer have to manage both short- and long-term side effects and related costs over a long period of time. For some, their treatment will never end, and this has many layers of implications which need to be addressed.
While we all agree that as a society we need to do a better job of controlling health care costs, we also have to recognize that we need the flexibility to create an individual plan for a patient based on co-morbidities, genetic predispositions, and other individual biological and psychological factors. There continues to be the need for a much-improved model of patient-centered care where the patient is consulted, respected and regarded as key to the decision-making process.
We are staring down the road at 77 million boomers who will be experiencing a wide range of medical conditions and serious and chronic illness. We are also staring down the road at a predicted shortage of health care workers during a time of growing need and demand. An educated and empowered patient who is involved in the process and trained to be his or her own best advocate has the potential to be one of the most powerful tools in the health care toolbox. Welcoming patients into the conversation could be -- I dare say -- revolutionary as we face these uncertain years ahead.