Bending the Health Care Cost Curve: Lessons from an Iowa Chicken Farmer
What can we learn about how to transform health care and "bend the cost curve" from a man raised on an Iowa chicken farm, with a Ph.D. in mathematics and physics who helped change our perspective of "made in Japan" from one of derision to one of emulation? Even though I had never heard of him at the time, he is the reason I have driven a Toyota for most of the past 20 years. William Deming (1900-1993) viewed industry, education and government as "systems". His idea was simple: improving quality (outcomes) will reduce costs, while improving productivity and market share. The focus was on quality not volume. In other words, doing the right thing pays. If the product of health care is "health", then how do we improve the quality of our health?
Clearly it is not by increased access to more care. [1] The four states with the highest health care expenditures, Texas, Louisiana, California and Florida, provide more care but have worse outcomes than other states in 25 metrics of quality of patient care. The Dartmouth Atlas Project found that in regions with more physicians, hospital beds, MRI scanners and more volume of services and care, health outcomes were worse and costs were up to twofold higher. More care--more spending--equaled more sickness, less access, and more patient dissatisfaction. In other words, poor value or unit of health purchased per dollar spent. We don't need more physicians. We need more physicians working with integrated healthcare teams doing the right things, paid in ways that incentivize health creation and "team work" rather than "piece work".
We need accountability for quality, cost, and outcomes. We need comprehensive tracking of metrics of value: improved biometrics, psychometrics, and econometrics. And we need true comparative effectiveness research between medications or procedures, and comprehensive lifestyle and environmental therapies, which are delivered by integrated health promotion teams.
An old New England farmer was asked, "How is your wife?" He answered in a way that all research institutions and policy makers should respond when evaluating any proposed treatment, "Compared to what?" The playing field needs to be leveled in CER (Comparative Effectiveness Research). [2] We need to compare lifestyle intervention and treatments that address the cause of diseases with medications or procedures. Lifestyle treatments are perceived not to work because all doctors know that patients don't change if you tell them to eat better and exercise more. Unless you give patients the support, education and tools to change behavior, you won't see sustainable, significant change.
But in multiple randomized trials in heart disease [3] and prostate cancer, [4] intensive lifestyle treatment by integrated health care teams haven been proven more effective than currently used and reimbursed treatments. More importantly these changes improve health, quality of life, and even enhance gene expression through lifestyle changes. In other words, they provide value.
The present system of care is unsustainable and will NOT reduce the burden of chronic disease. We need to implement a new system of care that addresses the proven drivers of chronic disease (what we eat, how much we exercise, how we handle stress and environmental toxins) and their associated costs. A healthcare system designed to address these drivers of disease and cost doesn't exist for one simple reason: It is not reimbursed. We simply don't pay doctors or health care providers to do this.
Over the last year, I have participated along with others in healthcare reform through meetings with Senators, Congressmen and their staffers, testifying before the HELP committee, and meeting with key health care leaders at Health and Human Services and The White House. I have been struck by one thing. Everyone wants the same thing: To improve quality (better outcomes and health), provide universal coverage and reduce costs. The only confusion and disagreement is about how to achieve that end.
The focus has been largely on ways to improve the delivery model and financing for our current "products" - pharmaceuticals, procedures and surgery. In other words, to do the same treatments better. If these were the best available treatments, if they produced the best health, then, of course, payment for more of these services would improve outcomes and quality and reduce costs.
Unfortunately, the research points to a very different conclusion. Nonetheless, most healthcare professionals do what they know how to do - prescribe medicines and perform procedures. The more we do, the more we get paid, regardless of the outcome or quality of the product--health. Following the status quo this way, we do not get more health for our money. Though we spend more than twice as much as any other industrialized nation on healthcare, we rank nearly last in mortality and other metrics of health. How then do we create health?
Creating Value and Quality: A High-Science, Low-Tech Approach to Chronic Disease
Within the conversation in Washington and the media, in proposed policies and bills, there is a conspicuous absence of one simple idea. If we want to improve the product of health care, namely, good health, then we must incentivize treatments that create health. What may startle many in the health care debate is that the research points to a very surprising fact.
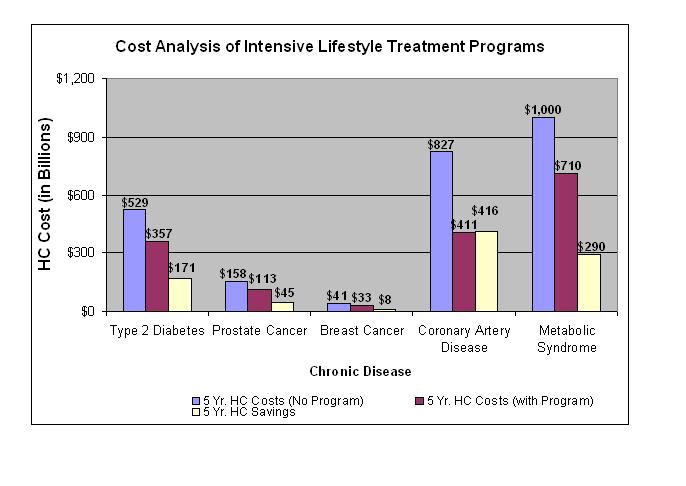
A high-science, high-touch, low-tech, low-cost treatment is more effective for the top five chronic diseases (which account over 75% of healthcare costs) than our current approaches. Yet is it not taught in medical schools, practiced by physicians, nor delivered in hospitals or healthcare settings. In fact, this treatment, if applied to all the patients with cardiovascular disease, diabetes, metabolic syndrome (obesity), prostate cancer, and breast cancer could reduce health care expenditures $930 billion over 5 years, [5] and result in a better "product"--higher quality at reduced costs. William Deming would be proud.
What is that treatment? It is intensive lifestyle intervention for chronic disease delivered by integrated health care teams paid for "team" work, not "piece" work. However this "treatment" is often incorrectly framed as prevention. Improving diet, exercising, and managing stress are seen as soft, yet under the lens of hard science, the evidence points to these as better strategies not only for prevention of disease before it has occurred (primary prevention), or preventing recurrence or exacerbation (secondary prevention), but also for lifestyle interventions as a better TREATMENT for existing chronic disease. This re-framing from lifestyle as prevention to treatment is necessary if we are to develop a mechanism to create a better product--health.
This is personal, not just academic. My stepfather died this year from complications of diabetes and cardiovascular disease. He had the best medical, pharmaceutical, and surgical care available, yet had very poor health and functioning. The evidence has shown no reduced mortality for cardiac bypass or angioplasty in diabetics. [6]
Yet, because we do what we know, and what is paid for, he had a cardiac bypass after chest pain. A post-operative infection of his sternum with MRSA (an antibiotic resistant staph bacteria) lead to a month in the intensive care unit, plastic surgery to repair the chest defect, and "mini-strokes" following bypass surgery, which led to memory loss or "pre-dementia", [7] and a protracted recovery from hospitalization requiring months of home care. The surgery, and subsequent medical therapy with blood pressure medication, cholesterol-lowering medication, and blood thinners, did not give him a very good product - quality of his health and life. In fact, he continued to be sedentary, craved sugars and refined carbohydrates, and decline rapidly physically and mentally. The cost of his medical care in the last years of life exceeded $400,000.
Yet how much "health" did that expenditure purchase? I would say it lead to a defective product and purchased no "health" at all. He was not offered a treatment that would have cost less than 2% of that, and would have likely created infinitely more value through better outcomes and enhanced quality of life. It should be our right to have access to proven treatments that provide better value for the individual and for the healthcare system. This shift must be made if we are going to significantly impact our chronic disease epidemic and the frightening convergence of the GDP and health care cost curves.
That is why we need a mechanism within healthcare to stimulate quality based on improved outcomes through the use of the best available data that addresses the upstream drivers of chronic disease. We must offer a treatment to address the causes of disease, not only send a patient to surgery, or prescribe poly-pharmacy. This is no longer a luxury, but a necessity to reverse this epidemic of chronic disease and costs.
Take Back Your Health
On August 6, 2009, Senator Ron Wyden [D-Ore] introduced new legislation, the "Take Back Your Health Act" (S. 1640) that will pay for intensive lifestyle changes as treatments, not just prevention, for these conditions as a complement to regular medical care. This legislation was co-sponsored by Senator John Cornyn (R-Tex) and Senator Tom Harkin (D-Iowa). Dr. Dean Ornish, Dr. Mike Roizen, and I consulted on this legislative language.
"This is a groundbreaking bill, based on the proven idea that lifestyle changes can improve the health of those with chronic disease if people stick with a program that has that goal in mind," said Senator Wyden. "The Take Back Your Health Act gets doctors and patients invested in the success of treatment, since doctors won't be paid unless their patients actually get better."
"This legislation will provide seniors who have chronic diseases with the care coordination, training, and support necessary to make and sustain intensive lifestyle changes that have been clinically proven to beneficially affect or even reverse the progression of many chronic diseases," said Senator Cornyn. "I'm pleased to join with my colleagues in a bipartisan fashion and will continue pushing for common-sense solutions to our health care system."
"The health reform debate is not about continuing the status quo, but about changing our health care system and the medicine we do," Senator Harkin said. "This legislation will change the medicine Medicare does by reimbursing health care professionals for proven programs to address disease, including coronary heart disease, diabetes, and some forms of cancer, through intensive lifestyle change. Health reform is about giving individuals more choices and individuals should be given the option to engage in a lifestyle treatment program instead of surgery and pills."
This bill is now working its way through Washington. Collective advocacy is needed to enact this long overdue strategy for creating quality not quantity in health care.
Here is what it would provide:
1. Intensive lifestyle treatment programs for heart disease, diabetes, metabolic syndrome, breast cancer, and prostate cancer (and, potentially, other chronic diseases as well), reimbursed at competitive bundled rates for team care that would incentivize wide adoption by healthcare institutions and professionals.
2. Personalized treatment plans delivered by integrated health care teams including physicians, and health care professionals trained in nutrition, exercise, stress management, and psychosocial support. This may include, but would not be limited to, registered dietitians, exercise physiologists, behavioral therapists, health coaches, and psychologists.
3. Individual and group sessions of up to 72 hours over the course of a year for the development of a personalized treatment plan and sustainable behavioral and lifestyle change.
4. Annual tracking and analysis of cost outcomes and payments linked to accepted biometrics and psychometrics.
5. Patient rewards to foster further health-oriented behaviors.
This would encourage development of treatment methods and applied nutritional science and behavioral therapies that result in the best outcomes and value.
This legislative mechanism in the health reform bill from Congress, or a regulatory mechanism through Health and Human Services must provide a small opening for intensive lifestyle treatments to take hold in medical care. It will be a lever for catalyzing change through simulating innovation for integrated healthcare teams for chronic disease management, the creation of the infrastructure for sustainable behavioral change, and payment for outcomes and quality, not volume. It will also reinvigorate primary care and drive the transformation of existing health care institutions, medical schools, postgraduate education, and insurers to meet the demand for interventional lifestyle treatment services for chronic disease. It will support shared responsibility, self-care and participatory medicine as well as changes in communities, and corporations that enhance lifestyle change. It will support the development of health information technology solutions to coordinate care, measure outcomes and costs, enhance research and facilitate whole systems medicine rather than automating our current model of care. It will support the development of a wellness- and health-based economy rather than one based on sickness and obesity. With one small change, one small lever, our sick care system could be transformed into a health care system.
References
1. http://www.dartmouthatlas.org Health Care Spending, Quality and Outcomes, February 27, 2009
2. Volpp KG, Das A. Comparative effectiveness--thinking beyond medication A versus medication B. N Engl J Med. 2009 Jul 23;361(4):331-3
3. Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, Sparler S, Armstrong WT, Ports TA, Kirkeeide RL, Hogeboom C, Brand RJ. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998 Dec 16;280(23):2001-7.
4. Ornish D, Magbanua MJ, Weidner G, Weinberg V, Kemp C, Green C, Mattie MD, Marlin R, Simko J, Shinohara K, Haqq CM, Carroll PR. Changes in prostate gene expression in men undergoing an intensive nutrition and lifestyle intervention. Proc Natl Acad Sci U S A. 2008 Jun 17;105(24):8369-74.
5. 17. Cleveland Clinic estimates for Take Back Your Health Act of 2009
6. BARI 2D Study Group, Frye RL, August P, Brooks MM, Hardison RM, Kelsey SF, MacGregor JM, Orchard TJ, Chaitman BR, Genuth SM, Goldberg SH, Hlatky MA, Jones TL, Molitch ME, Nesto RW, Sako EY, Sobel BE. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med. 2009 Jun 11;360(24):2503-15.
7. Newman MF, Kirchner JL, Phillips-Bute B, Gaver V, Grocott H, Jones RH, Mark DB, Reves JG, Blumenthal JA; Neurological Outcome Research Group and the Cardiothoracic Anesthesiology Research Endeavors Investigators, Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med. 2001 Feb 8;344(6):395-402.
Mark Hyman, M.D. practicing physician and founder of The UltraWellness Center is a pioneer in functional medicine.