Matt, a 35-year-old sales executive, considered himself successful -- at least in his work. Divorced and the father of an 8-year-old daughter, Matt spent a lot of time on the road, so much so that he said, "I think of airports as my office." He was as "connected" as anyone I knew and was capable of hosting complex meetings online while texting his daughter and waiting to board a flight home.
Matt's work life was also stressful, due in large part to "The Great Recession." Though he'd managed to maintain his sales performance, he told me that it now took a lot more time and effort to do so. It was that stress to which he attributed increasing difficulty sleeping through the night, as well as what he described as a low-grade depression. "I wake up thinking about everything I have to do. Work used to be fun, but it just hasn't been as much fun as it was three years ago," he told me when we first met.
When Mark went for his biannual physical, he mentioned his troubled sleep, said that he didn't seem to have as much energy as he used to, and that he'd been feeling "a little depressed." He also talked a little about his pressures at work. The doctor told Matt that what he was describing were all signs of depression. He recommended that Matt seek out some short-term counseling before they considered medication.
"It's All In My Head"
At the outset of our first session Matt again laid out his symptoms: trouble sleeping through the night, a loss of energy, and what he termed low-grade depression. Then he dropped the real reason he thought he was there: "I believe my doctor thinks this is all in my head, which is why he suggested I see a therapist." I asked Matt what he thought. He shrugged and said he thought he was just getting a bit worn down.
"Not In Your Head"
Over our next couple of meetings I filled in the picture of Matt's lifestyle, covering issues such as his relationship with his daughter, his hobbies and interests, his social life and his drinking patterns. That last item is what first caused my ears to perk up a bit. Not that it made me think that Matt was an alcoholic, because he wasn't. However, Matt turned out to be one of a group of people who I eventually came to think of as almost alcoholics.
What I learned was that over the past three years -- and apparently in response to increased performance pressures at work -- Matt had gone from someone who might have a beer or two, mostly on weekends, to someone who now drank two or three beers a night -- plus an occasional cocktail or two -- just about every day except on those days when his daughter visited with him, which given his extensive business travels amounted to no more than five or six days a month.
Connecting the Dots
Many diseases (including alcoholism) are characterized by "prodromal" signs that often appear long before the symptoms that formally define the diagnosis. Connecting the dots and recognizing the significance of these prodromal symptoms can be difficult. As an example, consider that increasing difficulty doing mental arithmetic calculations can be a prodromal sign of Alzheimer's -- a sign that can be easily overlooked. So it is with alcohol.
When almost alcoholics like Matt come to my office it is usually not for help with what they see as a drinking problem. They may be having trouble managing a teenage child. Or they may complain that their marriage seems to be troubled by too much fighting and too little sex. Sometimes they come in, as Matt did, because they've been feeling depressed or anxious for a long time, or have been suffering from chronic insomnia, decreased energy, and depression.
One of the prodromal signs of a developing drinking problem is disruption of a person's "sleep architecture." They may fall asleep easily (which may in fact be why they drink), but because of the alcohol they do not get sufficient deep sleep. And since it is during deep sleep that the brain rids itself of toxins, they wake up feeling tired instead of refreshed. Over time this chronic fatigue can contribute to precisely the kind of low-grade depression that Matt complained of.
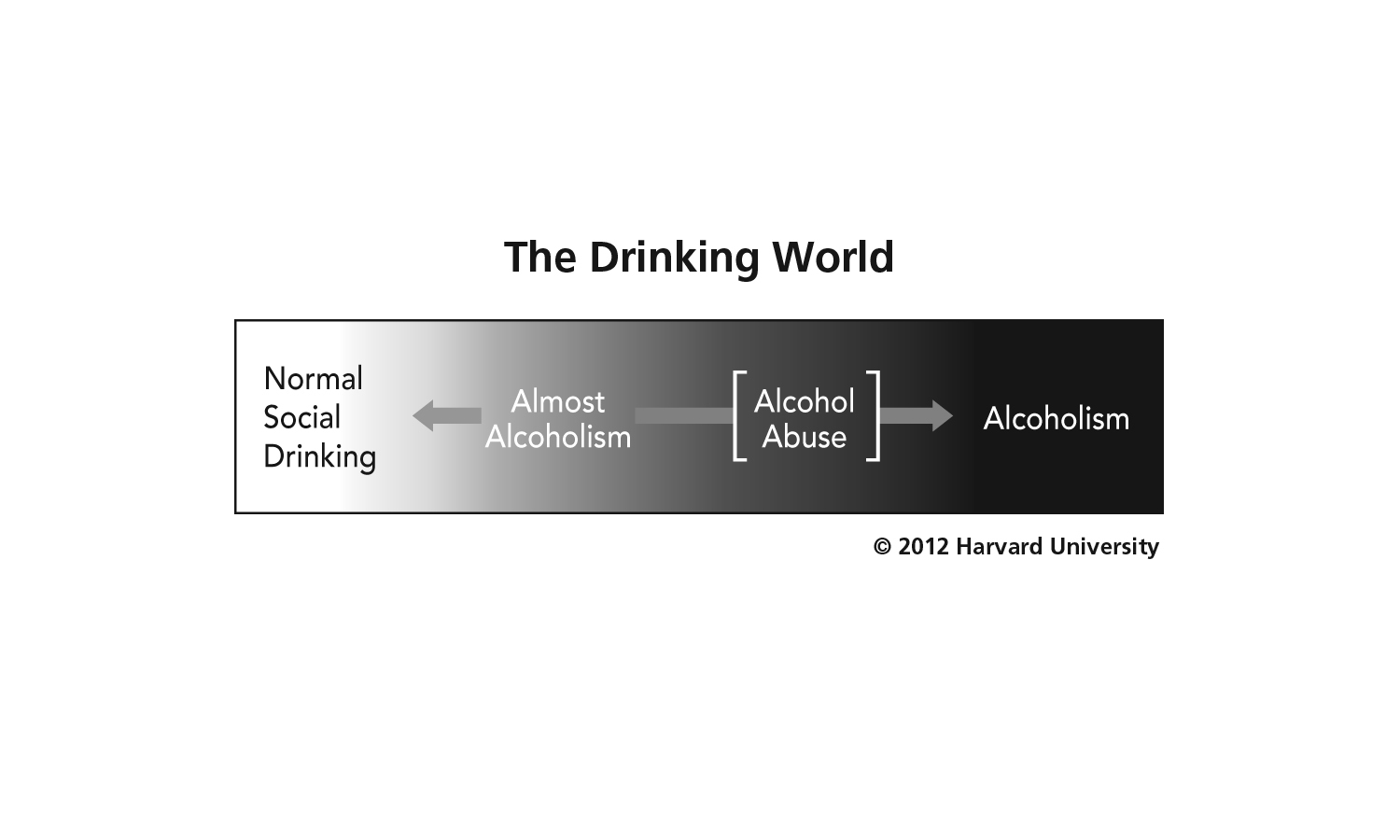
The challenge that I faced would be to convince Matt that his physical symptoms were in fact a prodromal sign -- that he had moved from being an occasional drinker into what I call the almost alcoholic zone, depicted in the diagram below:
I knew only too well from experience how defensive men and women can get when you try to make such a connection. They often jump to the conclusion that I'm calling them an alcoholic, when in fact I am not. What I am suggesting is that their physical symptoms are not "all in their head." Nor are they signs of some severe mental illness. They are prodromal signs of a developing drinking problem, though not necessarily signs of alcoholism.
I had gotten a release of information to talk to Matt's doctor, and I did just that. I explained my diagnosis and said that I would be sharing it with Matt. His doctor was very supportive and said that he would call Matt and ask him to come in for a follow-up appointment.
It's been over a year, and I still meet with Matt once a month or so. He still drinks, but limits himself to a couple of cocktails, beers, or glasses of wine a day, and only on weekends. Moreover, he's now sleeping well, has regained his energy, and no longer feels depressed. When we meet we talk about other things, like a new relationship he has. He's told this woman about his hazardous experience with drinking. He jokingly refers to our occasional sessions as his "insurance policy" against slipping into the almost alcoholic zone again.
Matt's condition -- being an almost alcoholic -- afflicts untold numbers of men and women, especially in a society like ours that encourages drinking. As such it may contribute in unrecognized ways to many conditions that are misdiagnosed as either psychiatric or medical in nature. Health and mental health practitioners need not see an alcoholic behind every symptom in order to recognize that there are indeed prodromal signs that may be evident years before a patient's drinking might be "diagnosable." Being open to that, and being able to help a patient connect the dots between prodromal signs and drinking, could spare many patients a great deal of suffering and possibly prevent more serious conditions from emerging.
For more by Joseph Nowinski, Ph.D., click here.
For more on addiction and recovery, click here.