There are two critical time gaps in joint injuries.
The first is the interval from when a joint is injured to when arthritis sets in. The second is from when arthritis sets in to when you are considered old enough for artificial joint replacement surgery.
For the knee, shoulder and ankle injuries that I've treated, these gaps have ranged from years to decades. But as we move into the 21st century, those gaps are looking very different.
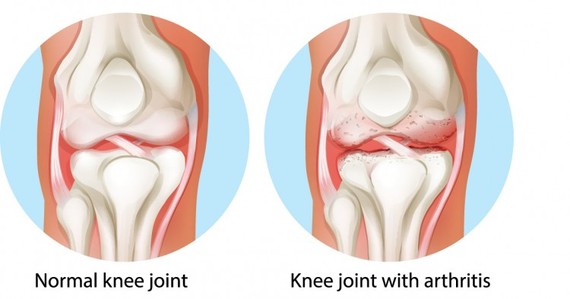
Let's first look at them historically, starting with gap number one. In the past, when a significant cartilage injury occurred, the damaged cartilage was either ignored or removed. Those removal procedures -- called meniscectomy for removing the knee joint meniscus, and chondroplasty for shaving away the articular cartilage -- left the joints with poor shock absorption. [1] The remaining cartilage surfaces wore out quickly, deforming the underlying bone. This in turn stimulated the formation of osteophytes (bone spurs), leading to instability of the joint. [2] This was especially true when key ligaments (such as the ACL in the knee joint) were also torn, leading to further degradation. [3-10]
Arthritis -- the wearing away of the cartilage and the deformation of the underlying bone--occurred almost universally after cartilage was removed. [3-10] The gap in time before arthritis set in was often silent. Many people, especially pro athletes, assumed they were healed, and returned to high levels of impact sports. Not until late in their careers did they realize they were faced with decades of joint pain.
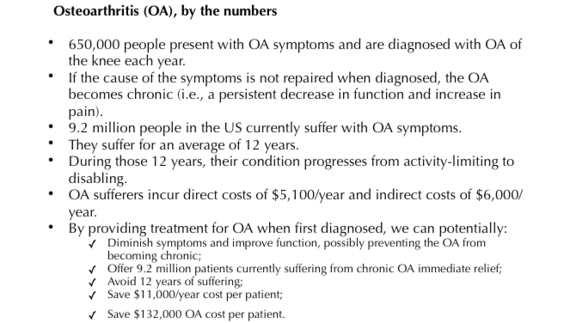
The second gap is the time between when the arthritis has become symptomatic -- with pain and loss of range of motion of the joint -- and the time at which joint replacement is recommended. Joint replacements are generally not advised before the age of 65 because (a) they only last a couple of decades, (b) they are nonreversible, and (c) up to 50 percent of patients with full knee joint replacements still have pain 10 years later. [11] Patients were therefore told to rest their knees, limit their activities, lose weight and take arthritis pain medications until they were 65. Tough advice for a 30 year old former pro athlete, or even for an active weekend warrior!
Today, we can "mind the gaps" differently. There is excellent long-term data suggesting that when the joints are injured, repairing or replacing the missing cartilage in combination with stabilizing the damaged ligaments returns many people to active sports. [12] This is achieved with less pain and better function scores, and without accelerating arthritis formation. Ten- to 20-year outcome studies now show that current cartilage replacement techniques, such as meniscus replacement and articular cartilage paste grafting, provide long-term relief both for healthy knees (when first injured) and for the arthritic knee. [12] The arthritic knee is thus able to delay or even avoid artificial joint replacement for decades.
For the ankle and shoulder there is significantly less data, but individual patient experiences have been encouraging. Cartilage replacement for the hip, unfortunately, is not yet available.
So mind the gap! Don't delay repairing or replacing injured critical tissues. And don't just rest and wait. An active lifestyle promotes health and productivity. The science of biologic joint replacement is advancing rapidly, and now offers much better solutions than, "just live with it."
REFERENCES:
1. Roos, H., Laurén, M., Adalberth, T., Roos, E. M., Jonsson, K., & Lohmander, L. S. (1998). Knee osteoarthritis after meniscectomy: prevalence of radiographic changes after twenty‐one years, compared with matched controls. Arthritis & Rheumatism, 41(4), 687-693.
2. Altman, Roy D., James F. Fries, Daniel A. Bloch, John Carstens, Derek Mb, T. Cooke, Harry Genant et al. "Radiographic assessment of progression in osteoarthritis." Arthritis & Rheumatism 30, no. 11 (1987): 1214-1225.
3. Simon, David, Randy Mascarenhas, Bryan M. Saltzman, Meghan Rollins, Bernard R. Bach, and Peter MacDonald. "The Relationship between Anterior Cruciate Ligament Injury and Osteoarthritis of the Knee." Advances in orthopedics 2015 (2015).
4. P. Neuman, M. Englund, I. Kostogiannis, T. Fridén, H. Roos, and L. E. Dahlberg, "Prevalence of tibiofemoral osteoarthritis 15 years after nonoperative treatment of anterior cruciate ligament injury: a prospective cohort study," The American Journal of Sports Medicine, vol. 36, no. 9, pp. 1717-1725, 2008.
5. E. Tayton, R. Verma, B. Higgins, and H. Gosal, "A correlation of time with meniscal tears in anterior cruciate ligament deficiency: stratifying the risk of surgical delay," Knee Surgery, Sports Traumatology, Arthroscopy, vol. 17, no. 1, pp. 30-34, 2009.
6. N. Al-Hadithy, A. L. Dodds, K. S. N. Akhtar, and C. M. Gupte, "Current concepts of the management of anterior cruciate ligament injuries in children," The Bone and Joint Journal, vol. 95, no. 11, pp. 1562-1569, 2013.
7. A. G. Culvenor, J. L. Cook, N. J. Collins, and K. M. Crossley, "Is patellofemoral joint osteoarthritis an under-recognised outcome of anterior cruciate ligament reconstruction? A narrative literature review," British Journal of Sports Medicine, vol. 47, no. 2, pp. 66-70, 2013.
8. R. Z. Fu and D. D. Lin, "Surgical and biomechanical perspectives on osteoarthritis and the ACL deficient knee: a critical review of the literature," The Open Orthopaedics Journal, vol. 7, pp. 292-300, 2013.
9. A. C. Gelber, M. C. Hochberg, L. A. Mead, N.-Y. Wang, F. M. Wigley, and M. J. Klag, "Joint injury in young adults and risk for subsequent knee and hip osteoarthritis," Annals of Internal Medicine, vol. 133, no. 5, pp. 321-328, 2000.
10. H. Louboutin, R. Debarge, J. Richou et al., "Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors," Knee, vol. 16, no. 4, pp. 239-244, 2009.
11. Naudie, D. D., Ammeen, D. J., Engh, G. A., & Rorabeck, C. H. (2007). Wear and osteolysis around total knee arthroplasty. Journal of the American Academy of Orthopaedic Surgeons, 15(1), 53-64.
12. Stone KR, Adelson WS, Pelsis JR, Walgenbach AW, Turek TJ. Long-term survival of concurrent meniscus allograft transplantation and repair of the articular cartilage: A PROSPECTIVE TWO- TO 12-YEAR FOLLOW-UP REPORT. J Bone Jt Surg Br. 2010;92-B(7):941-948. doi:10.1302/0301-620x.92b7.23182.