By Angel Gurría and Michael Porter
OECD economies already spend nearly 10 percent of GDP on average on health care, and this will only rise as populations' age and treatment options improve. In the last decade, for example, knee replacements have doubled from 60 per 100,000 people to 120. The question is, are we getting our money's worth from all this spending on health care? Today, the surprising truth is that we have no idea. Health systems have long amassed vast amounts of data--how many patients were treated, what services were delivered, whether clinicians followed guidelines, and how much was spent. However, we lack the data that patients, clinicians and health systems need the most --the outcomes achieved for patients and how they feel about them. Outcomes are the actual results of care, and include clinical measures such as survival rates and the complications arising during treatment. However, the outcomes that matter the most to patients are often how care affects their functionality and quality of life. Was Mrs. Smith free of pain after her knee replacement? Did she regain full mobility? Can a stroke survivor go back to work? Can a teenager suffering from depression resume school?
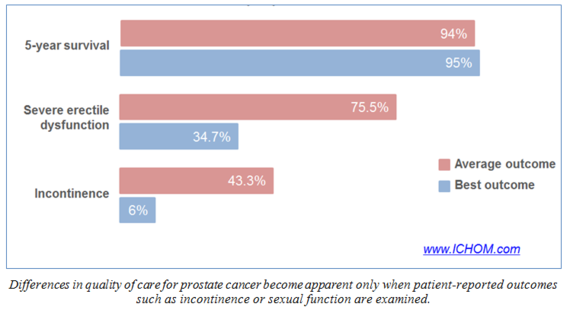
Collecting "hard" outcomes like mortality and complications is essential, and progress in measuring these is underway at the national and international level. But international benchmarks of health system performance in improving functional status and quality of life are completely absent. Clinical outcomes alone are not enough. For example, survival rates for men diagnosed with prostate cancer are quite similar across providers and across the main therapies, reflecting the nature of the disease. However, key quality of life measures (incontinence, bowel dysfunction, and sexual function) vary dramatically both within and across countries (see the Figure). Patients, clinicians and policy makers all stand to benefit hugely from these outcomes of health care.
Capturing functional and quality of life measures requires asking patients themselves-- whether they are better, or worse, or the same, on the things that matter most to their quality of life. Systematically using such patient-reported outcomes (often called PROMs) will revolutionize how we understand and improve the value of health care. Distinct, but complementary, to PROMs, patient-reported experiences (often called PREMs) measure aspects such as being given the opportunity to ask questions or be involved in treatment planning. Together, these patient-reported indicators will allow clinicians to make better choices about the care they provide and how to improve it; patients will be in a better position to decide what treatments are the most likely to benefit them as well as which providers do the best job in delivering good results; and policymakers will have the essential information they need to help make health care more efficient and effective, and get the most out of spending.
A few health systems are measuring PROMs. In the United Kingdom, for example, patient reported outcomes after hip and knee replacement are published on the My NHS website for every hospital. Internationally, though, comparable results from patient surveys are rare in OECD countries. Those patient surveys that do exist are often not comparable, and unrepresentative of the population as a whole. For hip replacement, for example, at least five different surveys are in use internationally. The result is that comparing performance across countries is virtually impossible.
We must fix this. We need a systematic and standardized approach to asking patients about the outcomes of their care that matter most to them, medical condition by medical condition. We must also measure overall primary care outcomes in managing people with multiple conditions. The OECD is already the most comprehensive source of comparable statistics on health and health systems in the developed world and has helped developing countries develop their information systems. But we can now take the next big step and take advantage of the internationally agreed upon sets of the most important outcomes by disease, including PROMs, that have been developed by the International Consortium for Health Outcomes Measurement (ICHOM). These already cover about half of the global burden of disease, and the number of diseases covered is growing rapidly. The time is now to harness the work of ICHOM, and others, to begin to systematically survey patient reported outcomes. The OECD is the natural forum to do this, and provide accurate and meaningful comparison of performance across countries.
Asking patients to assess the results of their care is perhaps the most important single step we can take to improve health care. It will change the culture and mindset among clinicians and throughout health systems. Getting this right will require political commitment at the highest levels. International organizations, governments, and clinicians must work together to better measure the impact of care on people's daily lives, and thereby assess the value that health systems create. This, after all, is the ultimate measure of success.
Angel Gurría is the Secretary-General of the OECD. Michael Porter is the Bishop William Lawrence University Professor at Harvard Business School and founder of ICHOM.
In January 2017, the OECD convened a meeting of Health Ministers and a High-Level Policy Forum, focused on people-centred care and the next generation of health reforms. www.oecd.org/health/ministerial