Dear Dr. Pat,
I'm 49 years old and had a diagnosis of HPV--human papilloma virus--four years ago, and my first abnormal pap smear at the same time. I had just ended a six-month relationship, and we didn't use condoms. My partner and I were both tested for sexually transmitted diseases before we had sex, and I had no HPV then. He told me that his doctor said he had no diseases, and he didn't want to use condoms.
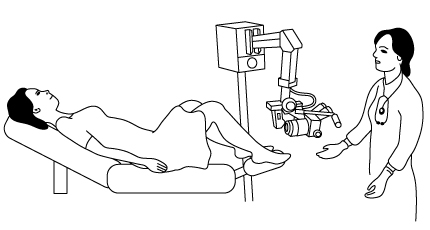
After the diagnosis of high-risk HPV and the abnormal pap smear, my gynecologist did a colposcopic exam [which allows the genital tissue to be evaluated through a magnification lens -Ed.]. This showed that I needed a larger part of the cervix taken out, to remove and diagnose the extent of the abnormal cells that had developed because of the HPV infection.
I had an uneventful LEEP cone biopsy in her office. [The LEEP procedure uses electrical current transmitted through tiny wires in a loop that removes the cone-shaped tissue from the cervix and cauterize the tissue left behind to control bleeding.] The pathology report showed only mild cell abnormalities (mild dysplasia), and also showed that the margins of the tissue were free of all precancerous cells--which my doctor said was very important.
For almost four years afterward, my Pap smears were normal, even though I was still HPV-positive. Three months ago, I had another mildly abnormal pap smear. The gynecologist said to repeat it in 10 weeks. That pap smear was slightly more abnormal. The doctor explained that, in order of severity, cervical dysplasia is mild, moderate and severe, followed by carcinoma in situ [early cancer that had broken through the cell walls], and then invasive cancer. At that point, I had CIN2, moderate dysplasia. The colposcopic exam was repeated and the biopsy report from the outside of the cervix showed moderate dysplasia. The biopsy from the endocervical canal [the passage leading from the cervical canal into the body of the uterus] was normal.
The gynecologist recommended that I have a hysterectomy to remove the entire uterus and cervix, leaving my ovaries in place. She stressed that the HPV that I have is high-risk and that removing the cervix with a hysterectomy would prevent me from developing cancer of the cervix. She pointed out that by doing this, I could forgo all the future cone biopsies that I will most likely need.
I don't want a hysterectomy, and all the risks of the surgery, when the LEEP cone biopsy was so easy and it did remove the abnormal tissue for four years. I understand that this virus can cause cancer of the cervix, but it doesn't always. What are the risks of just having another cone biopsy at this time? What else can I do to be proactive in finding abnormal cells before cancer develops, without having a hysterectomy?
Margaret
Dear Margaret,
You are certainly an informed patient and you ask very important questions. Communication between a patient and her doctor are crucial to the choice of surgical procedures. It is part of our informed consent process.
Colposcopy is done to improve the diagnosis and to help the surgeon create a treatment plan. When the pap smear is abnormal on more than one occasion, with a positive test for high-risk HPV, and the colposcopic exam is either normal or inadequate (where not all of the areas of the at-risk zone of the cervix are visualized), then a cone biopsy is the next diagnostic step. Patients need to understand that the cone biopsy is nearly always diagnostic, and hopefully therapeutic. By that, I mean that the abnormal cells are microscopic, and the surgeon has a general idea of how much of the cervix to remove during the performance of a cone biopsy, but sometimes the margins are not free of dysplasia. There is no way to prevent this.
In your case, the cone biopsy done by the LEEP method, which uses cautery to cut out the tissue, showed normal margins, free of abnormal cells. This was the right procedure for the mild dysplasia that you had at the time. If you now choose to have a second cone biopsy instead of a hysterectomy, do discuss the option of having the cone biopsy performed with a scapel instead of a LEEP procedure. This surgery is performed in an operating room, not a doctor's office.
Gynecologists call this procedure a cold knife cone biopsy to differentiate it from a LEEP cone biopsy. The margins of the surgically removed cervical tissue are easier for the pathologist to evaluate, because the cautery used in a LEEP procedure literally fries the tissue at the place where the tissue is cut away. The cold knife cone biopsy procedure is not done as often now, unless a decision to forgo a hysterectomy is to be based on careful pathology review of the tissue, or if there's evidence of cervical dysplasia inside the endocervical canal.
If you choose to have a cone biopsy, it will be important that the pathologist reports that there is no early cancer and that all the margins of the removed cervical tissue are free of abnormal cells. If either of these conditions exist, then you will need more extensive surgery. If the cervical margins are free and you have only cervical dysplasia, you should have a pap smear every three months for the next year, as long as all of those pap smears are normal. At that point, your gynecologist may suggest a pap smear every six months.
HPV under a microscope
As long as you remain HPV-positive you have an increased risk for more than cervical cancer. You are also at risk for vulvar cancer, which includes the labia and perineum (the area between the vaginal opening and the anus), and peri-anal, anal and vaginal cancer. There is growing awareness of some kind of association of the human papilloma virus and mouth, tongue and throat cancer. At this point there are no recommendations for HPV screening of the oral cavity for any woman who has HPV of the genital or anal area. However, it seems prudent for all women who have persistent high-risk HPV to ask their dentists to evaluate their mouths carefully at each visit. In addition, women with HPV should be aware of the need to have further evaluation of the oral cavity if there is a persistent growth anywhere in mouth or throat, new and persistent hoarseness, or difficulty swallowing. Speak to your gynecologist about whether you should have both an anal HPV test and an evaluation of the anus for areas of abnormal cells.
Even when a hysterectomy is performed and the cervix is removed, the HPV remains in the body, unless the immune system can clear the infection. You will need pap smears of the vagina every six months, even when the cervix has been completely removed.
Certainly, you need to be a responsible patient. Never miss a pap smear. Always get the report and discuss it with your doctor. And do discuss with your gynecologist these suggestions for monitoring other areas of the body where HPV can cause cancer.
Your story points out the dangers of not using condoms in any new relationship. Men are not tested for HPV as part of general STD testing. The general way that a man finds out that he may be infected with this virus is when he is told that a woman with whom he has had sexual contact has developed this infection. And he may never tell another potential partner.
Best,
Dr. Pat
Patricia Yarberry Allen, director of the New York Menopause Center, is a gynecologist affiliated with New York-Presbyterian Hospital and a board-certified fellow of the American College of Obstetrics and Gynecology. She is a spokesperson on women's health, and the publisher of Women's Voices for Change.
Also posted at Women's Voices For Change.