
When the Supreme Court made their final ruling about the constitutionality of the Affordable Care Act (ACA) on June 28, 2012, it was decided that individual states have the right to choose whether or not they want to expand Medicaid in 2014. With most public attention focused on the individual and employer mandates, the Medicaid expansion ruling did not take center stage. However, the SCOTUS decision was actually quite a game changer. Governors of each state are now tasked with making this major decision on the behalf of their residents.
A little Background Information
The ACA includes plans to expand Medicaid throughout the country to low-income Americans making up to 133 percent of the federal poverty level ($15,282 for individuals and $31,322 for a family of four). Five percent of household income is disregarded, which effectively raises the eligibility level to those making 138 FPL.
Why Expand Medicaid in the First Place?
The Medicaid program does not currently cover many low-income adults. In order to qualify, a person must meet the financial eligibility requirement and belong to one of the following groups: children, parents, pregnant women, people with severe disability, and seniors. This leaves out the large demographic of non-disabled adults with no children.
According to a report released by the Kaiser Family Foundation, if all states choose to expand, state Medicaid spending nationally would rise by $76 billion from 2013 to 2022 (less than a 3 percent increase), while federal Medicaid spending would increase by $952 billion (26 percent). Coverage could be expanded to 21.3 million individuals by 2022.
Between 2014 and 2016, the costs of the expansion will be picked up by the federal government in full. After that, the fed's contribution gradually decreases until it reaches 90 percent in 2022; it will remain at 90 percent thereafter. While the long term contribution from the fed is substantial, some states have indicated that even paying for 10 percent of the Medicaid expansion costs would severely hurt their state budgets.
State Responses
Some states have expressed interest in participating in a modified form of expansion; only extending benefits to working age, childless adults earning up to 100 percent FPL. The Obama administration has made it clear that there will be no compromises. In order to receive Medicaid expansion subsidies, a state must fully comply with the rules.
While there is no official deadline for states to decide, most governors have already announced whether or not they will expand. No Democratic states have turned down the expansion; governors from both sides of the aisle have announced plans to take advantage of it.
The argument could be made that states with higher rates of uninsured residents have more to gain by expanding Medicaid. Is this having any influence on the decision making process? The chart below shows where the states with the most uninsured residents stand on the issue as of now:
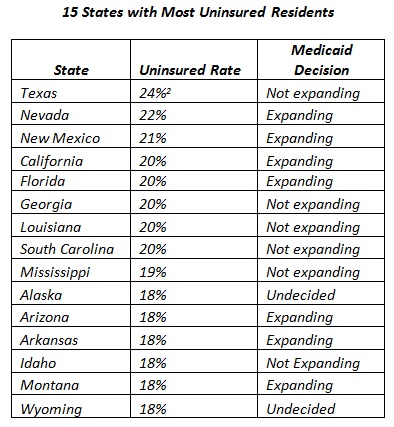
The official announcements from governors will continue to trickle in. As of March 6, 2013 a total of 14 states have declared that they will not participate in a Medicaid expansion and a total of 24 definitely will participate.
